In the interview below two members of Peaches Patient Voices describe their experience of getting involved with womb cancer research. Carol and Danni talk to Dr Louise Wan, Gynaecologist, BGCS RCS Specialty Lead for Gynae Cancer Studies.
To see these three women laughing and joking away on a Zoom call, you’d be forgiven for thinking that they were long lost friends. What they share is their passion for research than can make a real difference to people with womb cancer.
Danni was diagnosed with stage 3 womb cancer in October 2019 and completed treatment in May 2020. Despite, completing her treatment she feels the journey is definitely not over. She continues to deal with the late effects of the surgery and radiotherapy and coming to terms with how her body has changed and how different she feels.
Carol, sitting halfway across the country in her home in the North of England, was finally diagnosed in 2017. She recalls how daily tasks had become challenging and how she couldn’t even enjoy holidays because she was so worried about bleeding in someone else’s bed. At work, she was worried about standing for long periods of time as she would flood when she sat down but still didn’t feel that she had a valid enough reason to take time off. Her diagnosis came as a huge shock to her, and she recounts leaving the clinic room feeling numb and in sheer disbelief.
Louise is a gynaecologist and a long-time womb cancer researcher. She works with people like Carol and Danni every day. Their struggles have inspired her to research how health care workers can support people with womb cancer better; right the way through from their initial investigations to adjusting to life after treatment.
They tell their stories about the power of working together.
Why did you get in touch with Peaches Patient Voices?
Louise – My research is about how to provide patients and their loved ones with the information and support that they need to make decisions about their care. As people with womb cancer come in all different shapes, sizes and from different walks of life, I needed to find patient partners who reflected the diversity of the womb cancer community. One of my local specialist nurses suggested I contact Peaches Patient Voices. It is a great initiative as it provides a single point of contact for researchers like me to find people who have already expressed an interest in being involved in research. From the very start, they supported me in planning my patient involvement approach and I have been blown away by how responsive they were.
Danni – For me, it is so important to use my experience to contribute to any work that is being carried out in womb cancer. I have lived experience, like many other women, and I have to put that to some use. It helps me make sense of what I have been through as well. You don’t want horrible things to happen to you, and I don’t believe they happen for a reason. But I do believe that you can take something horrible and use it for good.
Carol – There is not enough awareness about this cancer. I see more and more people joining the support group that I am a part of everyday. I had never even heard of it before my diagnosis, and this has to change.
Why is shared decision making important in womb cancer?
Louise – In 2015, I coordinated the James Lind Womb Cancer Alliance project. We produced a top ten of the shared womb cancer research priorities that patients, clinicians, and researchers wanted addressing. Amongst these was “What are the psychological issues surrounding diagnosis and treatment of endometrial cancer and what interventions might be helpful?” As a doctor, I’ve seen so many people who have really struggled to come to terms with their diagnosis and life after treatment. This spurred me on to find ways to try to make this journey easier. Shared decision-making approaches are one way this could be done. They have been found to reduce treatment related distress, improve patient experience and mean that patients are more likely to engage fully with their treatment plan. There hasn’t been any research in this area in womb cancer specifically, so I want to see if people with womb cancer could benefit too.
Danni – I knew a little bit about the concept of shared decision making in my work as a Dementia Advisor and I was interested to see how it could be applied in the context of treatment options for womb cancer. I didn’t struggle with my treatment decision, but I do feel it would have been helpful to have had more information about the stage of cancer I had and why this led to the treatment that was offered and more importantly, deeper discussion and insight into possible (and probable!) long term effects of the treatment.
Carol – What interested me about the project is that the clinicians are finally listening to what patients want addressing. I wanted to understand the treatment and the impact it might have on me but there was no one around that I felt I could ask. I also did not know the questions I needed to ask. I wanted to be more aware of outcomes, quality of life, where to seek advice but also feel safe, confident, heard, and involved with whatever I chose. Having all of the above at the time of diagnosis I feel, would have made my journey a little less turbulent.
What did participating actually involve?
Danni – There was a helpful introductory webinar where Louise explained the concept of shared decision making and her research in this area. It was apparent straight away that she was open and receptive to our views and really reflected on the application of shared decision making in the context of womb cancer.
Louise – I wanted to get views about my plans to design a patient decision aid that would help close the gap between a person’s needs to hear about what treatment involves and the impact of potential side effects and their doctors focus on helping that person live as long as possible. So, after the webinar, we held a follow up workshop to start working on what that might look like.
Carol – Prior to the workshop, I received a welcome package in the post. I was so curious when I received a notebook, a mock decision-making booklet and Play-Doh… yes Play-Doh. Obviously as you can imagine I couldn’t wait to join in and I wasn’t disappointed. I was amongst a lovely group of ladies; all of whom had amazingly strong voices and who felt safe, comfortable, and confident to share their experiences.
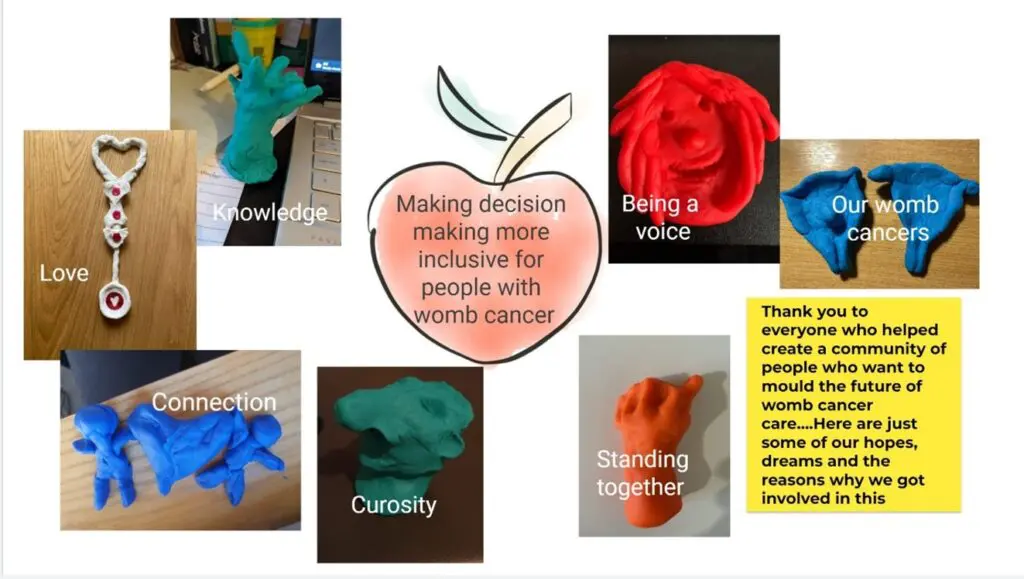
Various Play-Doh creations produced during the research project.
Do you have any tips for people thinking about being involved in a research project for the first time?
Carol – This is an excellent opportunity for us all to be heard and to finally have a say on how best to approach our own needs. Being part of this research project has allowed me to voice my experiences and to be part of bringing change to future patients that are being given this life changing diagnosis
Danni – Take the opportunity to use your experience for something good! You are a key element of any research as you have the lived experience and can help the researchers create a better world for people who will go through what you did.
Louise – Don’t be afraid to speak up! Having people with lived experience involved means that whatever we produce will be much more likely meet your needs and to be taken up by the NHS.
Any words of advice for researchers wanting to get patients involved in research?
Danni – From a patient’s perspective, please use us! There will of course be some patients who feel they can’t or don’t want to contribute. But there will be plenty who can and do!
Carol – The researchers in this project I feel have hit the nail on the head, I mean engagement with Play-Doh. Oh, what fun…I realised though I wasn’t very artistic.
Louise – Have fun! Stay curious! Patients are invaluable partners in designing and energising your research. Plus, when else can you legitimately get the Play-Doh out, laugh until you cry and still call that work?
Find out more about Peaches Patient voices.
Originally published May 2022
Updated November 2024


